Written by Brandon Okey. Mina Draskovic, B.Psy., reviewed this content for accuracy.
When people physically dependent on a drug discontinue its use, withdrawal symptoms can hit hard.
From nauseating physical effects such as vomiting, headaches, and tremors to depression and mood swings, withdrawal is a grueling process. In severe cases, trying to tough it out alone can be extremely dangerous or even life-threatening.
With proper medical care and social support, you can weather withdrawal safely. It’s a challenging but crucial first step on the road to recovery from addiction. With compassion and care, our drug addiction treatment center can help ease your discomfort.
This is a place to truly reset your life onto the right path. I learned such great healthy habits to live by. The staff are AMAZING so caring and friendly. I consider everyone I met at Ardu family. I truly hope the person looking for an amazing place to begin their new journey starts here.
Drug addiction is a complex disease that affects people from all walks of life. Reasons for drug use are different for each person: many turn to substance abuse to self-medicate pain, trauma, mental health issues, or other inner turmoil. Though it may start with a choice, over time it changes the brain’s chemistry and becomes compulsive, often despite negative consequences.
The most commonly abused drugs include:
If you or a loved one struggles with addiction to any substance, healing is possible. Reach out today to learn about treatment options at Utah rehab center and take the first step toward recovery.
If you’re addicted to drugs, your body and brain are dependent on the presence of the substance. When you stop using it, your entire system can react harshly. The severity of withdrawal symptoms and duration of the detox depends on the type of drug used.
Withdrawal from opioids brings on flu-like effects. Cardiovascular effects such as hypertension and arrhythmias are common as the heart is destabilized. The imbalance in the nervous system caused by alcohol or addiction to benzodiazepines results in frequent convulsions, tremors, and seizures. Gastrointestinal issues prevent proper intake, so nutrition, hydration, and electrolyte levels suffer. Every cell and organ system is sent into distress when the body and the brain are denied the drugs it has grown dependent on.
With depressants such as alcohol or benzodiazepines, you may experience life-threatening seizures if you stop abruptly. The overexcited nervous system must carefully return to baseline, which often requires medical supervision and medication. Stimulant withdrawal often plunges you into deep exhaustion and depression as the brain readjusts to normal dopamine levels.
Dopamine is a neurotransmitter that regulates motivation, pleasure, and mood. For example, in people with opioid addiction, the drugs flood the brain with dopamine, producing a “high.” The brain responds by reducing natural dopamine production and eliminating receptors, attempting to maintain equilibrium. This adaptation prompts the brain to become dependent on the drug to feel normal. If the drug is stopped, the starved neurotransmitter systems go haywire.
The rewarding effects of drugs of abuse, development of incentive salience, and development of drug-seeking habits in the binge/intoxication stage involve changes in dopamine and opioid peptides in the basal ganglia. The increases in negative emotional states and dysphoric and stress-like responses in the withdrawal/negative affect stage involve decreases in the function of the dopamine component of the reward system and recruitment of brain stress neurotransmitters, such as corticotropin-releasing factor and dynorphin, in the neurocircuitry of the extended amygdala. (Koob and Volkow)
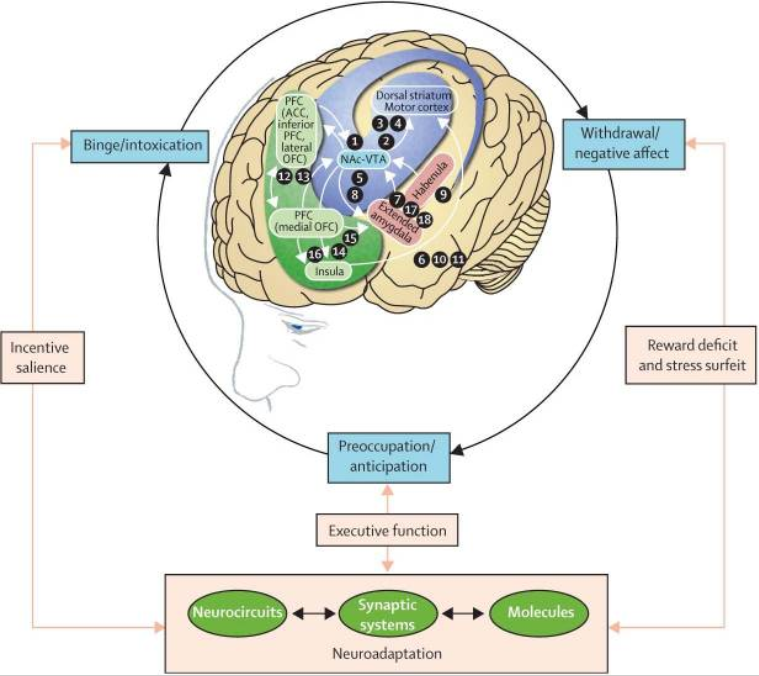
Koob and Volkow also suggest “decreases in the sensitivity of brain reward circuits to stimulation by natural rewards during the withdrawal/negative affect stage.” Remove the depressant drugs or the alcohol your brain needs, and your now over-excited nervous system misfires, potentially causing seizures and delirium tremens.
Alcohol withdrawal symptoms can be an excruciating ordeal, but a professionally supervised alcohol detox program might ease the burden and change your life.
Read more about the harmful effects of alcohol on the brain and what happens to your brain when you quit drinking.
Drug withdrawal can be an intensely difficult and uncomfortable process physically. Here are the most common physical symptoms of drug withdrawal:
As the body is denied the substance it had adapted to and grown dependent on, drug withdrawal takes a tremendous physical toll. But the troubles don’t stop there.
We’ve covered the physical symptoms of drug withdrawal, let’s now take a look at the psychological ones—which can be just as challenging.
When you’re getting off a drug after a long period of abusing it, your brain becomes confused and distressed. In addition to headaches, tremors, and impaired cognition, drug withdrawal also messes with you psychologically. They can persist long after the acute physical symptoms have passed, aggravating the challenge of your recovery from substance dependence.
The specific mental and emotional effects depend on the type of drug being abused, but the following are common psychological symptoms found across many types of drug withdrawal.
Psychological symptoms may linger but can be managed with lifestyle changes, counseling, social support, and time. With care, compassion, and proper medical treatment, both body and mind can return to a healthy balance.
Drug detox is an important first step in addiction recovery and returning your body to its normal rhythm. Detox should be followed by continued addiction treatment where you can focus on healing both body and mind.
We support you on your way to well-being as you process the psychological impacts of addiction and withdrawal. Our rehab program promotes a life free of addictive substances, allowing you to thrive and fulfill your full potential.
Kicking an addiction is tough—but an idea of what to expect can make the difficult detox journey a bit more manageable.
The withdrawal process can be divided into two phases: acute withdrawal and post-acute withdrawal.
The first 1–3 days since the last use are marked by great physical misery and intense cravings. Depending on the type of drug, this acute phase can last up to four weeks. Opioid withdrawal is shorter, lasting days to a week, but alcohol and benzodiazepines have more extended acute phases of 2–4 weeks.
During this time, it’s vital you are medically supervised and get the proper medical support.
Withdrawal is still mild at this point. You may notice some agitation or anxiety coming on, followed by the typical flu-like symptoms: headache, nausea, fatigue, and muscle aches.
Here’s where the symptoms become more obvious. Restlessness, sweating, and rapid heartbeat start to rear their heads.
The symptoms peak in intensity, with body aches, diarrhea, abdominal cramping, dilated pupils, racing heart, and sleep disruption striking hard.
After acute withdrawal resolves, post-acute withdrawal syndrome sets in.
After the intense flu-like symptoms fade, your brain now has to completely heal from dependence and enter the post-acute withdrawal phase or post-acute withdrawal syndrome (PAWS). This extended period of drug withdrawal is plagued by psychological symptoms that can persist for weeks to months as your brain rebalances, though gradually resolving with time and healthy coping strategies.
Many experience PAWS as a rollercoaster ride of good days followed by bad days where they struggle with mood swings, cravings, brain fog, fatigue, and poor sleep. Over time, the good days start to outnumber the bad as the brain rebalances its chemistry.
In some cases, PAWS can persist at lower levels for 1–2 years.
PAWS often follows a timeline like:
PAWS can be discouraging, but using healthy coping strategies speeds progress. You can seek the help of your health care provider or a counselor who can provide support.
At Ardu, we offer inpatient and outpatient drug treatment services that can assist you through both the acute and post-acute withdrawal phases. Our compassionate medical team and therapists will help you manage symptoms and process any difficulties that arise during your recovery journey.
Our inpatient drug rehab services and intensive inpatient treatment, as well as residential treatment programs, allow the patients to live on-site for a period of time to receive intensive treatment and the support they need.
If you choose our intensive outpatient treatment, you don’t have to stay at our facility. Instead, your treatment involves appointments at our center where you receive medical and emotional support. Outpatient detox is recommended for those who have mild to moderate addiction, have a supportive home environment, and are at low risk of medical complications during detox.
How long you’ll spend dealing with the rollercoaster of withdrawal symptoms depends a lot on which substance you were taking. While the acute physical symptoms tend to resolve within days or weeks, psychological effects can stubbornly linger for some time after.
But recovery takes as long as it takes; it’s not a race. Here’s what you need to know:
With the right treatment plan and support network, you can set your own pace through the withdrawal process.
Different types of drugs require different ways to deal with withdrawal and detox. While quitting some substances may be harmless for most, if you abruptly stop using opioids or benzodiazepines can have disastrous effects.
Here are some of the substances we help you detox from:
Alcohol detox helps manage withdrawal symptoms that occur when you decide to quit drinking. Our medically supervised alcohol detox provides 24/7 monitoring and care in a tranquil, comfortable facility. We carefully taper medication dosages as the body stabilizes.
We also help you deal with the dangerous consequences of long-term alcohol addiction, such as alcohol withdrawal syndrome. This refers to the severe, potentially life-threatening symptoms that can occur when alcohol intake stops abruptly.
Once detox is complete, our alcohol addiction treatment program offers therapies and support systems to help you maintain sobriety. We offer a full medical detox facility, paired with holistic detox therapies, to help you kick alcohol addiction for good.
There are three common drugs that professionals use to treat opioid addiction. They are methadone, buprenorphine, and naltrexone. We use these drugs during opioid detox to lessen opioid withdrawal symptoms. Once the detox process is over, our opioid addiction treatment program will support your continued recovery.
Heroin is one of the most commonly abused opioids. If you or a loved one are struggling with heroin addiction, our heroin detox program can provide comprehensive care and support to help you achieve lasting recovery.
In addition to heroin detox, we also offer detox services for the following non-prescription and prescription opioids:
Prescription drug detoxification should be done under medical supervision, as it can be dangerous to abruptly stop certain prescription drugs. Tapering off the drug gradually, with medical guidance, is often the safest method. A comprehensive prescription drug addiction treatment program, which includes counseling and behavioral therapy, can help address underlying issues contributing to the addiction and support long-term recovery.
Some of the prescription drug detox programs offered at Ardu include the following:
Stimulant withdrawal is not usually associated with medical complications. However, patients with recent cocaine use can experience persistent cardiac complications, and seizures and persistent headaches could be a complication of stimulant abuse during cocaine addiction treatment.
At Ardu, we have highly-trained personnel who are skilled at assessing and treating potential medical complications of stimulant use. We also provide detox services for the following stimulants:
A THC-specific withdrawal syndrome occurs in some patients who are heavy users. At Ardu, we offer marijuana detox services to people who are in need of a safe and effective way to cleanse their bodies from marijuana, as well as marijuana treatment services for long-term marijuana rehab.
Patients going through detox often have medical health conditions, such as depression, anxiety, personality disorders, eating disorders, and porn addiction, that can impact their overall health and the detox process. These co-occurring disorders can exacerbate addiction and vice versa.
A 2014 study on detox, substance abuse, and mental health treatment in patients with a dual diagnosis concluded that:
“Targeting more comprehensive mental health, case management, and 12-step programs to dually diagnosed patients with a history of detox may improve mental health and criminal involvement status.”
A dual-diagnosis treatment program is the best form of addiction therapy for people with co-occurring disorders. During and after detox, our dual diagnosis services are focused on relapse prevention and personalized treatment, including mental health services and trauma therapy that aim to uncover the underlying causes of addiction and help you manage your mental health disorder.
At Ardu, we made sure that the rehab admissions process is simple and straightforward. Simply verify your insurance by visiting our insurance verification page, make sure we accept your insurance coverage, and you’re ready to start your journey.
Our goal is to provide a welcoming environment focused on your health and sobriety from your very first interaction with our compassionate team. We’re ready when you are to take that first step towards healing.
For more information about rehab, here’s a helpful list of things to bring to treatment.

Brandon Okey is the co-founder of Ardu Recovery Center and is dedicated to empowering people on their journey to sobriety.
Withdrawal symptoms tend to be strongest during the initial phase. The severity is influenced by factors such as the type of substance, duration of use, and individual differences. The first few days after discontinuation, known as the acute withdrawal phase, typically feature intense symptoms. This period is challenging, marked by physical discomfort, psychological distress, and an increased risk of relapse.
The most serious form of withdrawal is often associated with severe alcohol use and is known as “severe alcohol withdrawal” or delirium tremens (DT). This condition can be life-threatening, characterized by hallucinations, severe confusion, elevated heart rate, and other dangerous symptoms of withdrawal. It requires immediate medical attention, and the risk of complications underscores the importance of seeking professional help during withdrawal, especially for substances with severe withdrawal potential.
Withdrawal behaviors encompass a range of physical and psychological responses exhibited by individuals experiencing withdrawal. These may include restlessness, irritability, muscle pain (a common symptom of withdrawal), insomnia, and difficulty concentrating. In severe cases, people may engage in drug-seeking behaviors, such as craving the substance, in an attempt to alleviate the discomfort associated with withdrawal.
Social withdrawal is a common symptom during withdrawal and is characterized by a person’s avoidance of social interactions. This can manifest as isolating oneself from friends and family, neglecting responsibilities, and avoiding social activities. If you’re undergoing withdrawal, you may experience heightened anxiety and mood swings, which only contribute to your desire to withdraw socially.
Emotional withdrawal feelings are often linked to the neurochemical imbalances that occur when the substance is no longer present. These emotional challenges can persist throughout the withdrawal process and may contribute to the risk of relapse.
Emotional withdrawal refers to the emotional aspects of the withdrawal process. This can include intense mood swings, heightened anxiety, depression, and irritability. It’s important to address emotional withdrawal through a comprehensive approach, which includes psychological care, support from mental health professionals, and, in some cases, medications to manage mood symptoms.
When you stop drug use, it can have many different consequences, both physical and psychological. Physically, you may experience unpleasant withdrawal symptoms, ranging from mild discomfort to severe symptoms such as elevated blood pressure, rapid heart rate, muscle pain, and clammy skin. There is also a risk of dangerous withdrawal symptoms, especially with substances like alcohol and benzodiazepines, which may lead to life-threatening complications such as seizures or heart attacks.
Psychologically, you may face challenges such as drug cravings, depression, and anxiety. The discomfort of withdrawal can make it difficult to sustain abstinence, increasing the risk of relapse. Professional medical intervention is often necessary to manage withdrawal symptoms safely. Long-term consequences, such as the risk of relapse, underscore the importance of follow-up treatment, supportive care, and psychosocial interventions to address the underlying issues contributing to substance use disorders.
Koob, G. F., & Volkow, N. D. (2016). Neurobiology of addiction: A neurocircuitry analysis. The Lancet. Psychiatry, 3(8), 760. https://doi.org/10.1016/S2215-0366(16)00104-8
Timko, C., Bonn-Miller, M.O., Mckellar, J., & Ilgen, M.A. (2014). Detoxification History and 2-Year Outcomes of Substance Use Disorder Treatment and Mutual-Help Group Participation. Journal of Drug Issues, 44, 21 – 4.
How long does alcohol detox take?
What detox signs is your body showing?
What are the types of illegal drugs?
What drugs cause severe kidney damage?
What happens to your liver when you stop drinking?
What are the signs of heroin addiction?
What medication to use for mental health?