Written by Brandon Okey. Mina Draskovic, B.Psy., reviewed this content for accuracy.
Alcohol might make for a fun Friday night, but each drink packs a poisonous punch for your nervous system.
The neurotoxicity of alcohol triggers inflammation and oxygen deprivation, and disrupts signaling between neurons. The result? Brain shrinkage, wiring damage, and increased vulnerability to dementia.
Alcohol is notoriously bad for your brain, heart, liver, and other vital organs. Whether you’re sipping it casually over the weekends, or binge drinking regularly, alcohol can ruin your health.
Do you think it’s time for a change? Our alcohol rehab center is at your disposal. We’re here to help you break the cycle of alcohol addiction and take on alcohol detox with comprehensive treatment and support.
Neurotoxicity is the pathological disruption of the nervous system. This includes both the central nervous system (brain and spinal cord) and peripheral (nerves). It occurs when toxins induce biochemical changes and inflict damage to neuronal signaling, plasticity, and nervous system physiology.
In the long run, this can lead to:
Ethanol is the actual alcohol in alcoholic drinks, and it is toxic to your body. Its metabolites—byproducts generated when your liver processes ethanol—can also be harmful. One of these byproducts is acetaldehyde.
According to TellmeGen, “[acetaldehyde] is a hepatic metabolite of ethanol and the primary factor for the appearance of alcohol hangover and facial flushing. It is 20 times more toxic than alcohol and a possible carcinogen.”
Acetaldehyde and other alcohol metabolites may actually cause neuronal death. According to research, “alcohol was reported to decrease the number of neurons by increasing apoptotic cell death and reducing cell proliferation through prolongation of the cell cycle.”
Here’s how:
Chronic and heavy alcohol consumption can lead to permanent damage to the brain. Based on everything we know about the effects of alcohol on the brain, here’s what you need to know about how dangerous excessive alcohol consumption is:
If you recognize any of these symptoms of alcohol misuse in yourself, now might be a good time for a change. In our alcohol rehab center, you’ll find skilled professionals ready to help you every step of the way toward building a healthier, happier life in recovery.
Alcohol’s siege on the nervous system gradually erodes neuronal integrity and produces diverse symptoms of neurotoxicity. Subtle symptoms can develop into more severe deficits and lead to widespread brain and nerve damage.
Alcohol neurotoxicity signs may include:
Without intervention, alcohol’s neural effects can ultimately lead to cognitive and physical decline. When given the chance, your brain can actually reverse some of the damage caused by alcohol consumption.
If you think you may be suffering from any of these neurotoxic side effects, it’s never too soon to ask for help. Quitting is challenging, but with the right help, you or your loved one can regain control and heal the brain from alcoholism.
Alcohol’s assault on neural tissue decimates nerve cells via inflammation and oxidative stress, progressively severing brain-body communication pathways to induce pain, numbness, and motor dysfunction over time.
Alcohol gradually devastates the neural tissues and pathways that enable us to think, feel, behave, perceive, and function effectively.
If you think we’re overreacting, let’s take a look at the evidence.
Alcohol causes neuroinflammation that can damage brain cells and circuits—paving the way for alcohol-related brain damage.
Alcohol activates the brain’s immune cells (microglia) and causes them to flood neurons with inflammatory chemicals. According to research, “chronic alcohol consumption induced microglia activation and peripheral macrophage infiltration in the CNS, particularly in the hippocampus.”
A 2022 study revealed that “alcohol is also a notable activator of neuroinflammation, which over the course of repeated use may temper the anti-inflammatory responses of exogenous/endogenous cannabinoid signaling.”
Oxidative stress is the imbalance between free radical production and antioxidant defenses in the body. Free radicals, or reactive oxygen species (ROS), damage proteins, lipids, and DNA. Neurons are particularly vulnerable as these highly toxic molecules readily oxidize lipids and proteins that make up neural cell membranes and organelles.
Research shows that alcohol metabolism dramatically increases oxidative stress by generating acetaldehyde and ROS. People suffering from alcohol use disorder (AUD) seem to have “a higher concentration of CNS ammonia, mitochondrial damage, and oxidative stress caused by increased levels of reactive oxygen species in relevant brain regions.”
Read more about the detrimental effects of alcohol on DNA.
Exposure to ethanol breaks down myelin insulation around your nerve fibers (axons), slowing neural communication between your brain and body. You often first notice numb, tingly extremities or motor coordination going awry as the toxicity kills nerve fibers, setting the stage for alcohol-induced neuropathy.
Chopra and Tiwari suggest a few more reasons why heavy drinking causes your nerves to go numb. They state, “activation of spinal cord microglia after chronic consumption of alcohol…oxidative stress leading to free radical damage to nerves, release of pro-inflammatory cytokines coupled with activation of protein kinase C,” and other factors.
A 2016 study reveals that “neuronal degeneration in adult brain arising during chronic alcohol exposure is, or is likely to be, via ‘excitotoxicity.’”
Alcohol is a depressant. While acute alcohol consumption calms neural activity, chronic drinking episodes cause your brain to compensate by turning hyperactive. It does this by boosting the main excitatory neurotransmitter (glutamate) and suppressing GABA, the calming neurotransmitter.
When alcohol withdrawal kicks in, GABA and glutamate are imbalanced. The resulting glutamate surge provokes destructive rounds of excitotoxicity that can erode cognition over time.
Great things happen to your brain when you quit drinking. With professional support, commitment, and a little patience, you can come out with a healthier, happier, alcohol-free brain. Contact Ardu and start your healing today.
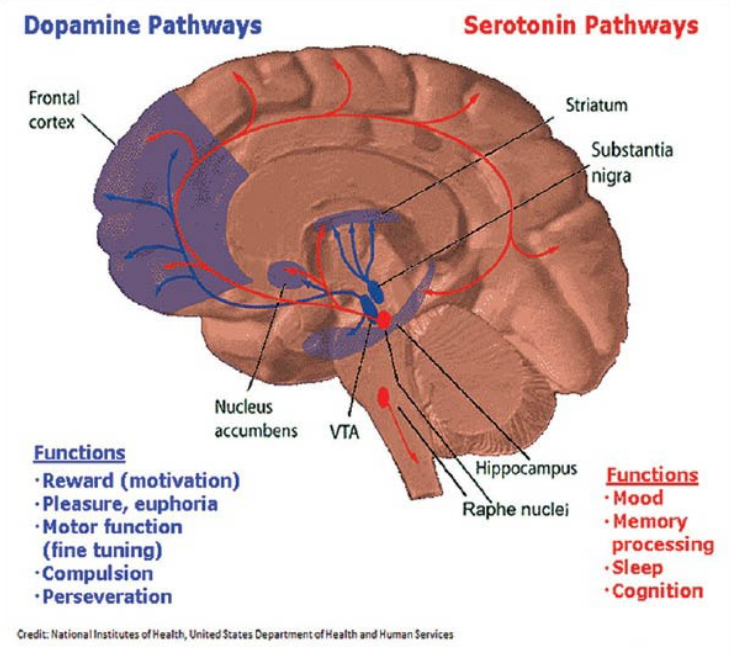
Speaking of neurotransmitters, alcohol has negative effects on all of them, not just GABA and glutamate. Excessive drinking alters levels of GABA, glutamate, dopamine, serotonin, and acetylcholine, which leads to communication disruptions between neurons.
According to research, alcohol hijacks the brain’s reward and stress pathways by altering neurotransmitter activity, which drives addictive behaviors that can eventually lead to alcoholism.
We’ve seen what alcohol does to GABA and glutamate. When it comes to serotonin-the neurotransmitter that is responsible for mood, sleep, and cognition-alcohol depletes its levels. It also reduces acetylcholine, the key neurotransmitter for attention, alertness, and memory formation. In contrast, binge drinking increases dopamine levels, overactivating the brain’s reward center and reinforcing addictive drinking behaviors.
Some people say alcoholism runs in their blood, but the true culprit may be alcohol’s ability to hijack your brain chemistry and foster addictive behaviors.
Your brain is malleable. It can reorganize and form new neural connections which are crucial for learning, memory, and adapting to changes. While the plasticity of our brains naturally declines over time, heavy alcohol exposure accelerates this decline.
Remember how chronic alcohol exposure downregulates glutamate and leads to excitotoxicity? Bell, et. al. suggest that “this excessive [central nervous system] glutamate activity alters synaptic plasticity, learning, memory, and stimulus conditioning associated with the development of alcohol and substance use disorders.”
Hawaiian researchers found that brain regions exhibit synchronized oscillatory activity, which means their firing patterns line up in a coherent way. This enables precise communication between the neural networks that drive your brain’s function. However, chronic heavy drinking disrupts synchronized communication between brain networks, inhibiting function.
Alcohol neurotoxicity can lead to diverse neurological conditions and cause damage to many parts of the central and peripheral nervous systems.
Booze is terrible for your liver as well as your nervous system. Do your best to limit your intake, or better yet, quit altogether. Our team of experts can provide support, guidance, and compassionate care as you take the important steps toward recovery.
Don’t wait until the damage becomes irreversible. Contact Ardu today.
Years of excessive alcohol consumption can cause significant alcohol-related brain damage. The extent of brain damage may depend on factors such as age, genetics, diet, and the severity of alcohol abuse over time.
Luckily, your brain is resilient and can repair itself once the heavy drinking stops. In fact, the human brain works best when there is no drinking involved. Our brains have a certain degree of neuroplasticity; neurons can regenerate and reconnect when given the chance.
Some alcohol-induced damage may be reversible with abstinence in the early stages of recovery. However, it may take longer periods of time to recover from the damage that excessive levels of alcohol consumption have inflicted upon your nervous system. Some long-term alcoholics may suffer more permanent effects.
Here’s what can happen to your brain when you stop drinking:
While substantial recovery is very difficult, dedicated treatment programs can help restore partial cognitive function after brain impairment from years of alcohol dependence. Our alcohol detox center provides individualized care, guiding you through the stages of overcoming addiction.
Alcohol-related brain damage is difficult to recover from, but not impossible. At our addiction recovery center, we specialize in helping people overcome alcohol addiction. Our team of skilled and experienced addiction specialists is here to provide the support, guidance, and personalized treatment you need to embark on your journey to recovery.
We believe in a comprehensive approach to recovery, so we strive to address not only the physical aspects of addiction but also the psychological and emotional aspects. We offer group therapy and individual therapy to all of our patients, as well as holistic treatment methods that delve into the underlying factors that contribute to alcohol addiction.
Remember, you don’t have to face addiction alone. We are here to support you every step of the way. If you’re ready to take the first step toward a healthier, alcohol-free life, reach out to us today.

Brandon Okey is the co-founder of Ardu Recovery Center and is dedicated to empowering people on their journey to sobriety.
Alcoholic neuropathy manifests physically as numbness, tingling sensations, nerve pain, and the progressive decline of motor function and control in the limbs. This can initially present as small gait abnormalities and a lack of coordination in arm, leg, and finger movements.
Neuroimaging studies reveal peripheral nerve damage and demyelination of motor neurons that disrupt signaling impulses to the muscle fibers. As motor neurons die off from alcoholic neuropathy, muscle weakness sets in, severely compromising balance and control of deliberate muscle movements. In extreme irreversible cases, alcoholic neuropathy may result in wheelchair dependence if damage to the nerves controlling lower body movement is severe.
The frontal lobes of the cerebral cortex and the cerebellum at the base of the brain are especially vulnerable to alcohol-related damage after extended periods of excessive drinking. Neuroimaging often displays pronounced shrinkage, dead cell zones, and significantly reduced metabolism of glucose and blood flow in prefrontal areas as well as the cerebellum.
Frontal lobe dysfunction manifests as cognitive impairment in executive functions like planning, as well as personality changes and behavioral disinhibition. Deficits in motor function are indicative of alcoholic cerebellar degeneration. The cerebellum normally coordinates detailed fine-tuning of movements, posture, and speech articulation, and also modulates cognitive faculties. Chronic long-term alcohol consumption inflicts gradual cerebellar Purkinje cell loss, resulting in the potential for severe loss of basic motor control and independence.
MRI and CT scan neuroimaging can reveal multiple signs of excessive alcohol use and related neurological diseases. The imaging studies may display shrinkage of entire brain regions and damage to subcortical white matter, as well as ventricular enlargement and neuron damage in areas commonly vulnerable to alcohol users. Such patterns, when correlated clinically with a history of prolonged alcohol consumption, can help confirm alcohol-related cognitive and motor function deficits.
There are several factors that affect the rate at which alcohol kills brain cells. These include the following:
Post-mortem autopsies of alcoholics consistently display shrunken brains and an overall loss of tissue mass with significantly fewer neurons in comparison to non-alcoholic individuals These range from almost 25% loss in key memory consolidation areas like the hippocampus, to a nearly one-third loss of volume with dead zones across subregions of the frontal cortex.
The frontal lobes located right behind the forehead are affected early and rather severely by the impacts of alcohol consumption. This is a result of their high sensitivity to neurotransmitter imbalances, even from low-dose consumption. This results from widespread disruption of delicate dopamine, serotonin, and GABA receptor equilibrium dynamics that are governed by frontal lobe networks.
Clinically, this emerges through some of the earliest signs: disinhibition, personality changes, and executive performance deficits. Toxic effects of alcohol consumption continue to target, compromise, and hijack limbic and reward pathways situated primarily in the prefrontal cortex regions.
Over longer periods of alcohol abuse, damage spreads to most brain areas, but the frontal lobes are among the first to be affected.
Exercise may be able to negate some degree of alcohol-related toxicity by increasing blood flow, neurotransmitter levels, and neurotrophic growth factor levels to regenerate neural networks.
However, this only remains possible for those early in the drinking stages, or those with limited damage from shorter periods of alcohol abuse. Years of severe chronic alcoholism are highly unlikely to be fully reversed. Substantial memory loss, as well as deficits in executive function and coordination, are virtually irreversible regardless of interventions.
If you decide to stop drinking, aerobic exercise provides real benefits by boosting neuroplasticity. It may help build around remaining pathways after alcohol has damaged major neural routes beyond repair. Working up a sweat won’t resurrect obliterated neurons from years of drinking, but it can strengthen neural regeneration.
There are certain vitamins and nutritional compounds that can help counteract some of the neuron-killing toxicity and inflammation alcohol triggers. A balanced diet rich in brain-protective foods forms a first line of defense. Beyond this, supplements such as vitamin B and magnesium act as receptor antagonists, blocking excitotoxic damage triggered when alcohol dysregulates neural receptors.
Antioxidants are always good to have in your system. Potent antioxidants such as resveratrol neutralize free radical reactions and may mitigate the loss of grey and white matter tissue microstructure seen in some chronic alcoholism disorders. Omega-3s nourish neuron cell membranes while B vitamins like B1 and folic acid aid molecular cleanup detail, promoting neural regrowth.
Alcohol-induced ataxia refers to difficulty with movement coordination, gait instability, and lack of muscle control caused specifically by alcohol damage to the cerebellum. For alcoholic cerebellar degeneration, it is possible to improve motor function and muscle coordination over an extended alcohol-free period.
However, the likelihood of regaining smooth independent gait and movement proficiency is still generally unlikely in people with a history of prolonged excessive drinking. This is especially true for those diagnosed at older ages where neuroplasticity has waned over time.
Partial recovery varies based on multiple factors:
Many things can be toxic to your nervous system and damage neurons. Some of the substances and factors that can to neurotoxicity in the nervous system include:
Acetaldehyde (Adverse effects). (n.d.). tellmeGen. https://www.tellmegen.com/en/results/pharmacology/acetaldehyde-adverse-effects
Lowe, P., Morel, C., Ambade, A., Iracheta-Vellve, A., Kwiatkowski, E., Satishchandran, A., Fűri, I., Cho, Y., Gyöngyösi, B., Catalano, D., Lefebvre, E., Fischer, L., Seyedkazemi, S., Schafer, D. P., & Szabó, G. (2020, October 9). Chronic alcohol-induced neuroinflammation involves CCR2/5-dependent peripheral macrophage infiltration and microglia alterations. Journal of Neuroinflammation. https://doi.org/10.1186/s12974-020-01972-5
Serrano, A., & Natividad, L. A. (2022, January 1). Alcohol-Endocannabinoid Interactions: Implications for Addiction-Related Behavioral Processes. Alcohol Research. https://doi.org/10.35946/arcr.v42.1.09
Coppens, V., Morrens, M., Destoop, M., & Dom, G. (2019, September 12). The Interplay of Inflammatory Processes and Cognition in Alcohol Use Disorders—A Systematic Review. Frontiers in Psychiatry. https://doi.org/10.3389/fpsyt.2019.00632
Chopra, K., & Tiwari, V. (2012, February 13). Alcoholic neuropathy: possible mechanisms and future treatment possibilities. British Journal of Clinical Pharmacology. https://doi.org/10.1111/j.1365-2125.2011.04111.x
Banerjee, N. (2014, January 1). Neurotransmitters in alcoholism: A review of neurobiological and genetic studies. Indian Journal of Human Genetics. https://doi.org/10.4103/0971-6866.132750
Bell, R. L., Sari, Y., & Rahman, S. (2019, January 1). Alcohol and Central Glutamate Activity: What Goes Up Must Come Down? Elsevier eBooks. https://doi.org/10.1016/b978-0-12-813125-1.00047-7
Fein, G. (2015). Neuroplasticity in Human Alcoholism: Studies of Extended Abstinence with Potential Treatment Implications. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4476599/
Tateno, M., & Saito, T. (2008, January 1). Biological Studies on Alcohol-Induced Neuronal Damage. Psychiatry Investigation. https://doi.org/10.4306/pi.2008.5.1.21
Daviet, R., Aydogan, G., Jagannathan, K., Spilka, N., Koellinger, P., Kranzler, H. R., Nave, G., & Wetherill, R. R. (2022, March 4). Associations between alcohol consumption and gray and white matter volumes in the UK Biobank. Nature Communications. https://doi.org/10.1038/s41467-022-28735-5
Oscar-Berman, M. (2003). Alcoholism and the Brain: An Overview. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6668884/
How much alcohol is too much to drink?
Are drinking habits a part of my personality?
Does alcohol accelerate normal aging?
How does alcohol dehydrate the skin?
Is alcohol bad for the kidneys?