Written by Brandon Okey. Mina Draskovic, B.Psy., reviewed this content for accuracy.
Alcohol wreaks havoc far beyond the morning hangover. Your drinking habits may alter your basic genetic building blocks, down to your DNA and cells.
Drink after drink, alcohol stresses vulnerable cellular structures— it attacks your DNA molecules to compromise genetic integrity, disables protective mechanisms inside cells, and ultimately triggers lasting changes that undermine your health.
If alcohol is damaging your health, it’s time to seek help. The decision to end alcohol dependency isn’t an easy one, but it truly is life-changing.
For those struggling with alcohol addiction, Ardu’s rehab center provides you with everything you need to kick your drinking habit to the curb.
I am very happy with the staff at Ardu and the whole detox program! Extremely caring people work at this place.
DNA (deoxyribonucleic acid) is the fundamental genetic blueprint of every individual. DNA molecules contain all the information needed to build and maintain the entire human body. This critical genetic code directs nearly every cellular process.
DNA regulates:
When DNA works properly, the body achieves peak performance. One of the major disruptors of DNA’s function is alcohol.
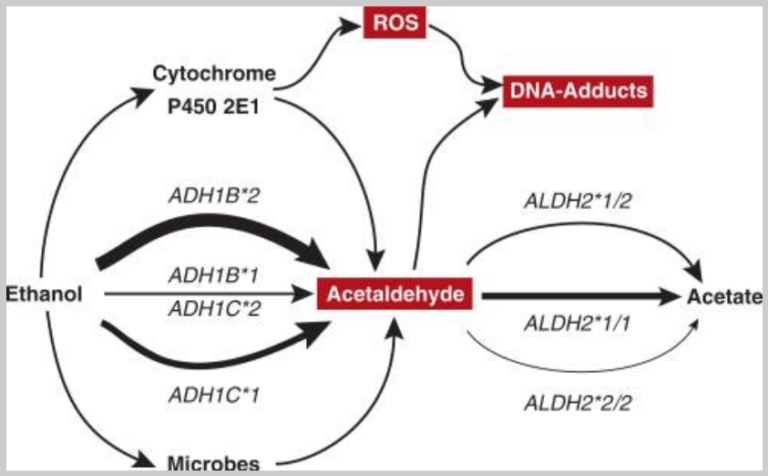
Ethanol (the “alcohol” in alcoholic drinks) physically damages DNA molecules. The damage doesn’t stop there: alcohol metabolism generates toxic DNA-damaging compounds such as acetaldehyde and reactive oxygen species (ROS).
Here are some of the most critical ways alcohol and its metabolites damage DNA:
Your body has innate mechanisms that repair this alcohol-induced DNA damage. However, heavy drinking downregulates this process and leads to an accumulation of DNA damage. A 2016 study revealed that “ethanol concurrently induced DNA [double-strand breaks], downregulated DSB repair pathway proteins, and increased apoptotic factors in hippocampal cells.”
The Fanconi Anaemia DNA repair pathway fixes the DNA crosslinks formed by acetaldehyde. Acetaldehyde can bind chemically to DNA molecules to create crosslinks between nucleotide base pairs. The FA pathway specifically fixes these DNA lesions by cutting out the damaged crosslinked segments and repairing the DNA strands.
Cells are protected against acetaldehyde-induced damage by DNA crosslink repair, which when impaired causes Fanconi anaemia (FA), a disease resulting in failure to produce blood cells and a predisposition to cancer. (Hodskinson, et. al.)
The more you drink, the less likely these mechanisms will work in your favor. But alcohol doesn’t only damage DNA at the very basic level. Heavy drinking compromises cellular and genetic integrity, triggering a dangerous chain reaction that disrupts everything from cellular communication to tissue function and ultimately whole-body homeostasis.
At the cellular level, alcohol’s bad for your brain, liver, kidneys, heart, skin, and other organs. Despite the negative health effects, many people struggle to say no.
You don’t have to struggle alone. The caring and supportive staff at our alcoholism treatment center can help you through the recovery stages, from alcohol detox to the sweet freedom from addiction.
Cells are your body’s basic building blocks. They are microscopic structures filled with specialized parts that enable them to grow, communicate, and fulfill unique roles. Tucked inside the nucleus (a cell’s center), DNA directs nearly all cellular operations to maintain their health and specialized function within the larger organism.
Your cells follow DNA instructions to:
Alcohol consumption directly impacts DNA molecules in the nucleus with toxic chemicals that tear at the strands and scramble codes. Your cells become disrupted and confused, so they are no longer sure how to fulfill their duties properly.
Cancer Research UK reveals that acetaldehyde damages the DNA within cells, leading to deadly mutation, irreversible genetic damage to the body’s reserve of stem cells, and increased cancer risk.
Let’s examine some of the ways alcohol disrupts cell function.
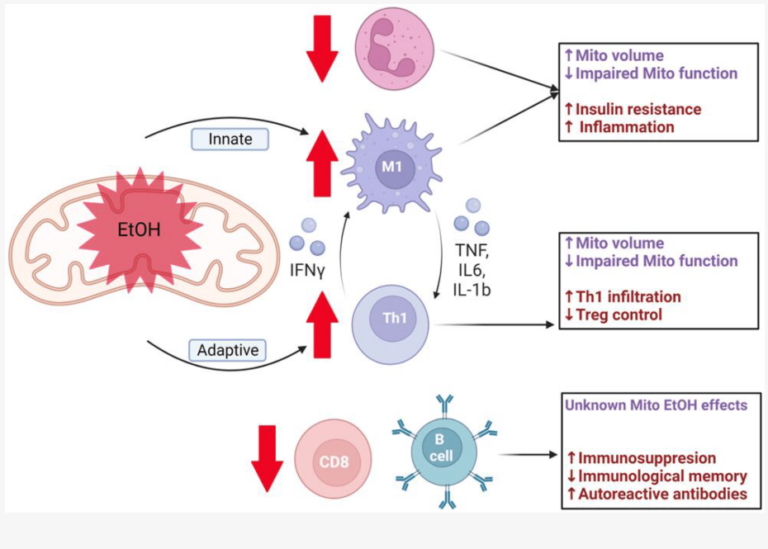
The first destructive step alcohol metabolites take is to increase inflammation throughout the body. Increased inflammation raises the number of free radicals and reactive oxygen species that wreak havoc on the cellular level
Oxidative stress is the imbalance between the body’s antioxidants and harmful free radicals. These volatile molecules contain unpaired electrons that damage proteins, membranes, and DNA through unchecked oxidation.
ROS can damage or cause complete degradation (i.e., peroxidation) of essential complex molecules in the cells, including fat molecules (i.e., lipids), proteins, and DNA. Both acute and chronic alcohol exposure can increase production of ROS and enhance peroxidation of lipids, protein, and DNA… (Wu and Cederbaum)
Membranes are the barriers that encase and protect your cells. They regulate the transport of material in and out of the cell to keep things running smoothly and allow communication signals to be received from the environment.
Research suggests that the membranes of animals treated with ethanol become stiffer. Ethanol increases the uptake of cholesterol or saturated fatty acids into membranes to reduce their fluidity and efficacy in protection, signaling, and communication.
Finnish researchers found that high concentrations of alcohol can change the membrane structure to change the shape of transmembrane proteins and disable their ability to transport materials.
Proteins and enzymes are complex molecules that adopt very specific 3D shapes to interact with other targets and carry out assigned duties within cells. When proteins lose their meticulous shape or “denature”, they’re left powerless to fulfill their specialized cell roles.
Herskovits, et. al. reveal that alcohol can disrupt the folded native form of proteins, causing denaturation. Alcohol essentially reshapes, misfolds, and deactivates pivotal proteins by interfering with the delicate hydrogen bonds and other forces stabilizing their anatomy.
Due to dysfunctional proteins, your cells are no longer able to carry out a host of other survival tasks.
Cells rely on regulated metabolic pathways to harvest nutrients and oxygen to power all operations. Glucose metabolism provides energy “fuel” in the form of ATP molecules. Adenosine triphosphate (ATP) is the key energy currency used by cells to drive critical cellular reactions.
Alcohol’s toxic metabolites impair nutrition. They disrupt each step in the processing of glucose and other nutrients by:
As a result, your cells are starved of energy sources and can’t carry out ATP-driven basic functions such as maintaining membranes, communicating, completing mitosis, repairing DNA damage, and more.
If you want to break the vicious cycle of alcohol dependence, our residential treatment can help you achieve and maintain your sobriety. We also provide nutrition therapy and counseling on how to repair cellular and DNA damage from alcohol abuse.
Read more about why nutrition is important during recovery.
Alcohol does more than slow or halt nutrient metabolism. It also disrupts oxidized nutrient molecules that produce ATP for energy.
Cellular respiration is the process cells use to convert nutrients into ATP. This metabolic process employs cell organelles and enzymatic pathways to unlock the stored chemical energy cells need to maintain their structure, communicate, repair damaged DNA, and complete other operations.
With respiration pathways blocked, cells are robbed of energy. No ATP means a crisis for powering membrane pumps, waste removal, DNA repair, and molecular synthesis—all the processes vital for cell survival.
Alcohol disrupts cellular respiration in the following ways:
…ethanol produces alterations in the mitochondrial structure and function of several organs, including liver, and heart…. These changes affect the mitochondrial function, decreasing respiratory rates and ATP levels, and might result in increased production of reactive oxygen species (ROS). (Manzo-Avalos and Saavedra-Molina)
The Medical University of South Carolina further explains that alcohol can lead to damage, degradation, and loss of mitochondria, all causing additional damage to cells.
Mitochondria are vital cellular organelles. These “powerhouses” of the cell convert oxygen and nutrients into chemical energy molecules that fuel all other cellular operations. They accomplish this through intricate structures within their membranes that shuttle electrons and harness their movement to drive phosphorylation.
Healthy mitochondria are essential for cells to carry out functions, communicate properly, remain structurally intact, and fix any damages that occur. After just one night of heavy drinking, ethanol can inflict serious damage to mitochondria.
Mitochondria also helps metabolize ethanol through the enzyme called aldehyde dehydrogenases (ALDH). ALDH converts acetaldehyde into acetate, a less harmful compound. When you consume alcohol at high levels over long periods, acetaldehyde builds up faster than ALDH can break it down. Manzo-Avalos and Saavedra-Molina suggest that this accumulates to toxic levels that directly damage mitochondria.
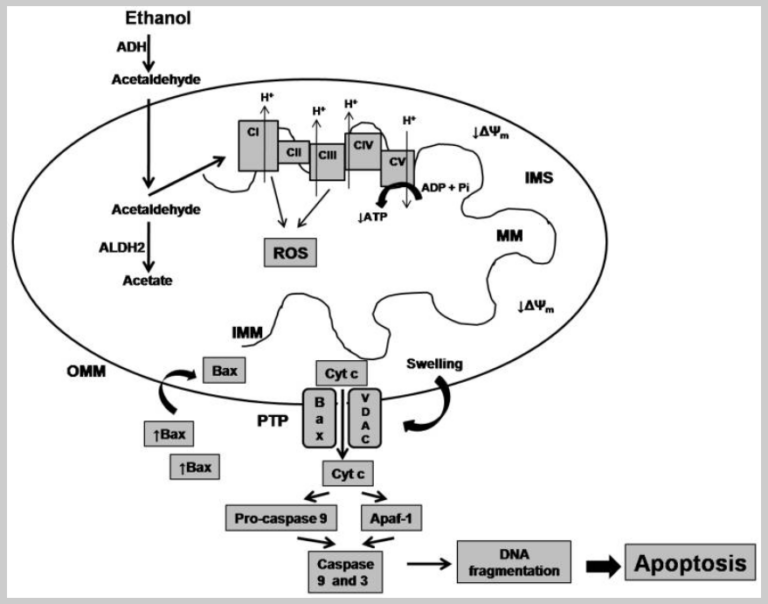
As you can see in the image, alcohol metabolism overburdens cell defenders, allowing byproducts to damage mitochondria and promote cellular self-destruction.
Alcohol is toxic at nearly every level of your body. (Read all about alcohol’s neurotoxic effects if you don’t believe us.) At the cellular level, alcohol and its byproducts directly damage the cell’s structural elements.
Here’s what you need to know about the way alcohol induces cell toxicity and ultimately death:
Alcohol can induce many forms of programmed cell death, or apoptosis, all of which play a crucial role in the progression of alcohol-associated liver disease. This means that alcohol’s toxic effects on your liver stem directly from its toxicity at the cellular level.
Heavy drinking also causes “multiple forms of cellular stress, including oxidative stress, hypoxia and endoplasmic reticulum (ER)-stress, resulting in activation of both intrinsic (mitochondrial) and extrinsic ([death-receptor mediated]) modes of apoptotic cell death.” (Miyata and Nagy)
Now might be a good time to stop drinking and prevent these damaging effects on your DNA, brain, liver, and other organs. Many people who stop experience severe withdrawal symptoms and, before they know it, unpleasant symptoms turn into alcohol withdrawal syndrome.
You don’t have to go through this alone. Contact Ardu and get the personalized treatment you need to embark on your journey to recovery.
From initiating DNA damage to influencing cellular signaling pathways, alcohol’s effects ripple through the microscopic realms, setting the stage for a cascade of physiological consequences. It affects virtually every organ in your body by impairing cellular regeneration and disrupting the finely tuned balance of tissue maintenance.
Here are some of the effects of alcohol on different tissues:
Are you sure you want to order another round?
Alcohol is a significant cancer risk factor. Its toxic metabolites damage DNA and cause chronic systemic inflammation that spurs uncontrolled cell growth and a whole lot of other mayhem. Research shows that even moderate alcohol consumption is linked to an increased likelihood of several types of cancer. A 2020 global study found that about 4.1% of all new cancer cases worldwide were caused by alcohol.
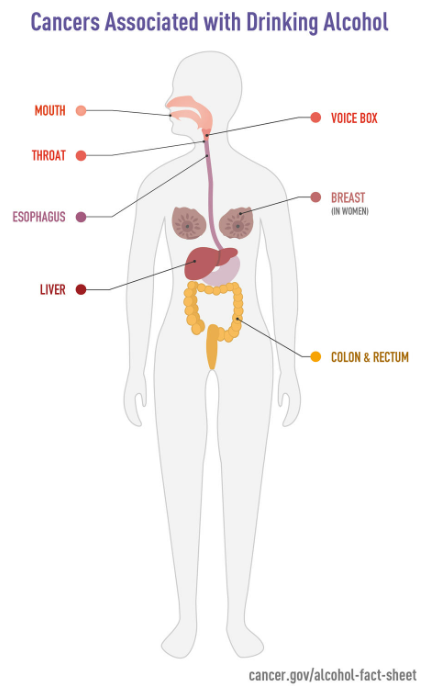
Alcohol contributes to cancer by damaging DNA and causing mutations. Acetaldehyde is a highly reactive and toxic compound that binds directly to DNA, forming DNA adducts. DNA adducts are unstable structures that can disrupt the normal functioning of DNA. They may lead to errors during DNA replication, causing mutations.
Acetaldehyde is carcinogenic in rodents and causes sister chromatid exchanges and chromosomal aberrations in human cells. The best-studied DNA adduct from acetaldehyde is N(2)-ethyl-2′-deoxyguanosine, which is increased in liver DNA obtained from ethanol-treated rodents and in white blood cells obtained from human alcohol abusers. (Brooks and Theruvathu)
Remember how chronic alcohol use disrupts mitochondrial function? Booze has the same effect on your immune cells, decreasing levels of protective cells and increasing pro-inflammatory immune responses. This contributes to a cancer-friendly environment.
Alcohol-related DNA damage may trigger the activation of oncogenes or the inactivation of tumor suppressor genes, further promoting carcinogenesis. Choi, et. al. revealed that chronic alcohol consumption diminishes genomic DNA methylation in the colonic mucosa, potentially providing a mechanism that enables alcohol to enhance the development of colorectal cancer.
Turn to Ardu Recovery Center and learn how you can stop binge drinking before it’s too late.
Through direct DNA damage and secondary impacts that erode genetic integrity, chronic alcohol exposure can chemically modify your genes and lead to mutations or cell death. A 2012 study concluded that “among those who drink heavily… the same genes may increase cancer risk by increasing levels of acetaldehyde in the tissues.”
Mutations disable normal safeguard genes or improperly activate growth genes and trigger excessive cell proliferation (cancer cell growth). By damaging DNA, alcohol can introduce errors that foster cancerous cell overgrowth, either by hampering natural tumor suppression or spurring increased activity of genes that drive cancer cells to divide uncontrollably.
Here are some of the main deleterious effects of alcohol on your genes:
Miles, M. D. found that “chronic heavy drinkers can tolerate alcohol without exhibiting obvious signs of impairment at doses that in other people would be incapacitating or even fatal.” This tolerance could arise due to changes in the expression of specific genes in the brain, one of the mechanisms through which the organism may adapt to chronic alcohol exposure.
The evidence is clear: heavy drinking chips away at your DNA over the years, allowing more diseases to take root. What’s more, alcohol changes your genes to increase tolerance and build dependence.
But the good news is that some alcohol damage can be undone. Sobriety lets your cells reboot and restore genetic integrity over time. You should start the sobriety journey now before alcohol use disorder or binge drinking over the weekends take a wrong turn.
So for your health and well-being, the best prescription is kicking alcohol fully so the body can reclaim homeostasis. Contact us today and start your recovery.
Research shows that genetics has a significant influence on the risk of developing alcoholism. The estimates are that between 40 and 60% of a person’s risk can be attributed to genetic factors. That’s why many people apply the disease model of addiction to alcoholism, in which alcohol addiction is often seen as a disease instead of a choice.
According to a 2022 study, specific DNA epigenetic signatures in brain reward regions may be associated with addiction susceptibility. Chronic exposure to addictive stimuli can lead to alterations in the epigenome, which can even be transmitted across generations, affecting the behavior of one’s children.
Of course, genes alone do not determine whether you’ll develop alcohol use disorder (AUD). Verhulst, et. al. confirm that alcohol use disorder is roughly 50% genetic, but claim that biology, genetics, and environmental factors all play a major role in addiction development for alcohol.
It can be difficult to recognize and acknowledge that you or a loved one may be struggling with addiction. Ardu Recovery Center offers a structured and supportive environment where you can receive medical care, counseling, and therapies to overcome your addiction and regain control over your life.
Anyone struggling with alcohol abuse or addiction is welcome in our alcohol addiction treatment program. Our recovery center is for people seeking help to overcome their alcohol addiction and restore physical and mental health. Our dedicated team of professionals is here to guide and support you in your addiction treatment process, laying the foundation for long-term sobriety and relapse prevention.
At our rehab center in Provo, Utah, our team specializes in helping those with dual diagnoses: addiction and concurrent health issues. We provide:
To enroll in an Ardu alcohol rehab program, contact us online or via phone (801-810-1234). We will do our best to find a recovery path that works for you during the detox process and beyond. For more information, read our admissions process page.
Getting proper treatment empowers you to manage alcoholism while implementing lifestyle changes to improve skin health. With compassion and expertise, we can help you achieve lasting sobriety and skin rejuvenation.

Brandon Okey is the co-founder of Ardu Recovery Center and is dedicated to empowering people on their journey to sobriety.
Alcohol can alter DNA methylation patterns by either hypermethylating or hypomethylating certain gene regions. In other words, alcohol can cause too many or too few methyl groups to attach to DNA, which incorrectly turns genes on or off by blocking or exposing the underlying genetic code to the cell’s machinery.
Studies reveal that alcohol increases methylation of genomic CpG sites in drinkers’ blood cells, more specifically, epigenetic changes associated with silencing gene expression. Over time, this differential methylation can deregulate key cellular processes contributing to carcinogenesis.
By increasing DNA fragmentation, alcohol can compromise sperm quality and fertility. Alcohol metabolism generates DNA-damaging ROS and acetaldehyde, while simultaneously crippling cells’ DNA repair systems that fix errors. One study found over half of alcoholic men had significantly fragmented sperm DNA compared to abstainers. This damage can also be passed down from fathers, increasing the risk of childhood cancers or congenital defects.
No single “alcohol gene” has been identified so far. Polymorphisms in genes involved in alcohol metabolism pathways such as ADH and ALDH are heavily implicated in the increased risk of alcohol addiction, as they influence the accumulation of toxic metabolites. Receptor genes impacting behavior and addiction such as GABA, opioid, and dopamine receptors also mediate genetic risk. On an epigenetic level, alcohol alters numerous gene expression profiles through DNA methylation and histone modifications.
While moderate drinking may have negligible genetic effects, heavy consumption above recommended limits causes measurable DNA damage. Studies reveal blood cells show tangible DNA fragmentation once drinkers exceed 3-4 drinks per day. Over the years, this genetic corrosion can enable disease without obvious symptoms thanks to increased tolerance.
Once you exceed those CDC-recommended limits of 2 drinks daily for men and 1 for women, alcohol starts eroding DNA integrity. Turns out our livers harness built-in alcohol digestion systems to safely metabolize some moderate intake through pathways utilizing handy enzymes like alcohol dehydrogenases (ADH).
But pound a few too many brews, and suddenly ADH and protective mechanisms get overwhelmed as byproducts. The cell-damaging acetaldehyde and DNA-attacking reactive oxygen species start accumulating faster than the body can clear or repair what they wreck.
Alcohol abuse can drastically lower testosterone. There are many mechanisms involved: direct testicular injury from ethanol, impedance of testosterone synthesis pathways, and others. A 2019 study found that chronic alcoholic men averaged a 37% drop in total testosterone compared to non-drinkers.
Both testosterone production and spermatogenesis seem to be affected by alcohol abuse in a dose-dependent manner: heavy drinkers are more likely to have a poor testicular function than moderate consumers.
Alcohol and its metabolites directly damage mitochondrial DNA and membranes through oxidative damage, interfere with ATP energy production, and disrupt the organelle’s ability to maintain cellular respiration. This leads to a shortage of energy needed for cells’ basic functions.
Ethanol and acetaldehyde have a particular affinity for the lipid membranes housing mitochondria. Alcohol chemicals embed right in mitochondrial membranes, warping their delicate folds and changing permeability. This structurally comprises the meticulous protein machinery responsible for churning out ATP energy molecules. What’s more, ethanol metabolism leaks dangerous ROS straight into mitochondria, oxidatively damaging the mitochondrial DNA itself.
Before you know it, the main powerhouses sustaining cellular activity grind to a halt thanks to serious apparatus damage and tanked ATP output. Without energy transfer abilities, cells quickly spiral into functional chaos. On top of the DNA mutations alcohol causes, its organelle sabotage is a brutally effective route to disrupting genetic integrity further.
Alcohol’s deleterious effects can cause mutations in genes. Multiple epidemiological studies tracking populations ranging from chronic alcoholics to risk drinkers reveal increased susceptibility across an array of alcohol-related cancers. Alcohol can cause DNA damage and mutations, leading to the activation of oncogenes or the inactivation of tumor suppressor genes, and promoting carcinogenesis.
Beyond genetic mutations, alcohol’s influence on DNA extends to aberrant DNA methylation patterns, as observed in studies tracking populations with different levels of alcohol consumption. These aberrant methylation patterns can contribute to the dysregulation of gene expression and genomic stability, further entwining alcohol with the complex landscape of cancer development.
The risk of breast cancer and colon cancer has been linked to alcohol consumption, emphasizing the importance of understanding the intricate molecular mechanisms through which alcohol exerts its influence on genetic integrity.
Alcohol can throw a bit of a wrench into the smooth process of DNA extraction, causing headaches for researchers. When we’re trying to pull DNA out of cells for analysis, excess alcohol in the mix introduces unwanted impurities like proteins, polysaccharides, and phenolic compounds. These uninvited guests mess with the purity and integrity of our precious DNA samples, making it harder to trust the results of our experiments.
To make matters trickier, alcohol can be a troublemaker during the lysis stages, causing the DNA to break into fragments and further muddying the waters for downstream analyses. So, researchers have to be savvy in adjusting their protocols to sidestep alcohol-induced obstacles and ensure their DNA extraction process is a clean and reliable affair.
Research shows a compelling relationship between heavy alcohol intake and an increased risk of cancers. Chronic alcoholism and heavy consumption are associated with a higher likelihood of developing hepatocellular carcinoma, neck cancer, and breast cancer. Alcohol-related CpGs—specific genomic regions affected by alcohol—have been identified as potential biomarkers for assessing cancer risk.
Studies have explored the impact of alcohol on DNA, revealing mechanisms such as the damaging effects of endogenous aldehydes and disruptions in DNA repair processes. People with hereditary breast cancer may face an elevated risk when combined with excessive alcohol use. The risk of colon cancer has also been associated with alcohol consumption.
Vijayraghavan, S., Porcher, L., Mieczkowski, P. A., & Saini, N. (2022, July 1). Acetaldehyde makes a distinct mutation signature in single-stranded DNA. Nucleic Acids Research. https://doi.org/10.1093/nar/gkac570
Poynter, J. N., Haile, R. W., Siegmund, K. D., Campbell, P. T., Figueiredo, J. C., Limburg, P. J., Young, J., Marchand, L. L., Potter, J. D., Cotterchio, M., Casey, G., Hopper, J. L., Jenkins, M. A., Thibodeau, S. N., Newcomb, P. A., & Baron, J. A. (2009, October 1). Associations between Smoking, Alcohol Consumption, and Colorectal Cancer, Overall and by Tumor Microsatellite Instability Status. Cancer Epidemiology, Biomarkers & Prevention. https://doi.org/10.1158/1055-9965.epi-09-0517
Suman, S., Kumar, S., N’Gouemo, P., & Datta, K. (2016, August 1). Increased DNA double-strand break was associated with downregulation of repair and upregulation of apoptotic factors in rat hippocampus after alcohol exposure. Alcohol. https://doi.org/10.1016/j.alcohol.2016.06.003
Hodskinson, M., Bolner, A., Sato, K., Kamimae-Lanning, A. N., Rooijers, K., Witte, M., Mahesh, M., Šilhán, J., Petek, M., Williams, D. M., Kind, J., Chin, J. W., Patel, K., & Knipscheer, P. (2020, March 4). Alcohol-derived DNA crosslinks are repaired by two distinct mechanisms. Nature. https://doi.org/10.1038/s41586-020-2059-5
McCarthy, A. (2021, April 12). Alcohol and cancer: This is how booze damages DNA inside cells. Cancer Research UK – Cancer News. https://news.cancerresearchuk.org/2018/01/03/alcohol-and-cancer-this-is-how-booze-damages-dna-inside-cells/
Wu, D., & Cederbaum, A. I. (2003). Alcohol, Oxidative Stress, and Free Radical Damage. Alcohol Research & Health, 27(4), 277-284. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6668865/
Goldstein, D. B. (1986, September 1). Effect of alcohol on cellular membranes. Annals of Emergency Medicine. https://doi.org/10.1016/s0196-0644(86)80120-2
Patra, M., Salonen, E., Terämä, E., Vattulainen, I., Faller, R., Lee, B. W., Holopainen, J. M., & Karttunen, M. (2006, February 1). Under the Influence of Alcohol: The Effect of Ethanol and Methanol on Lipid Bilayers. Biophysical Journal. https://doi.org/10.1529/biophysj.105.062364
Herskovits, T. T., Gadegbeku, B., & Jaillet, H. (1970, May 1). On the Structural Stability and Solvent Denaturation of Proteins. Journal of Biological Chemistry. https://doi.org/10.1016/s0021-9258(18)63111-4
Simon, L., & Molina, P. E. (2022, January 1). Cellular Bioenergetics: Experimental Evidence for Alcohol-induced Adaptations. Function. https://doi.org/10.1093/function/zqac039
Manzo‐Ávalos, S., & Saavedra‐Molina, A. (2010, December 21). Cellular and Mitochondrial Effects of Alcohol Consumption. International Journal of Environmental Research and Public Health. https://doi.org/10.3390/ijerph7124281
Problems in the powerhouse: Excessive degradation of mitochondria is the tipping point from normal alcohol metabolism to alcoholic liver disease. (2022, May 24). MUSC | Charleston, SC. https://web.musc.edu/about/news-center/2022/05/24/problems-in-the-powerhouse
Hoek, J. B., Cahill, A., & Pastorino, J. G. (2002). Alcohol and Mitochondria: A Dysfunctional Relationship. Gastroenterology, 122(7), 2049. https://doi.org/10.1053/gast.2002.33613
Miyata, T., & Nagy, L. E. (2020). Programmed cell death in alcohol-associated liver disease. Clinical and Molecular Hepatology, 26(4), 618-625. https://doi.org/10.3350/cmh.2020.0142
Rumgay, H., Shield, K. D., Charvat, H., Ferrari, P., Sornpaisarn, B., Obot, I., Islami, F., Lemmens, V., Rehm, J., & Soerjomataram, I. (2021, August 1). Global burden of cancer in 2020 attributable to alcohol consumption: a population-based study. Lancet Oncology. https://doi.org/10.1016/s1470-2045(21)00279-5
Brooks, P. J., & Theruvathu, J. A. (2005, April 1). DNA adducts from acetaldehyde: implications for alcohol-related carcinogenesis. Alcohol. https://doi.org/10.1016/j.alcohol.2005.03.009
Choi, S., Stickel, F., Baik, H. W., Kim, Y., Seitz, H. K., & Mason, J. B. (1999, November 1). Chronic Alcohol Consumption Induces Genomic but Not p53-Specific DNA Hypomethylation in Rat Colon. Journal of Nutrition. https://doi.org/10.1093/jn/129.11.1945
Edenberg, H. J., & Foroud, T. (2013, May 28). Genetics and alcoholism. Nature Reviews Gastroenterology & Hepatology. https://doi.org/10.1038/nrgastro.2013.86
Miles, M. F. (1995). Alcohol’s Effects on Gene Expression. Alcohol Health and Research World, 19(3), 237-245. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6875773/
Genetics of Alcohol Use Disorder | National Institute on Alcohol Abuse and Alcoholism (NIAAA). (n.d.). https://www.niaaa.nih.gov/alcohols-effects-health/alcohol-use-disorder/genetics-alcohol-use-disorder
Kaplan, G. J., Xu, H., Abreu, K., & Feng, J. (2022, January 25). DNA Epigenetics in Addiction Susceptibility. Frontiers in Genetics. https://doi.org/10.3389/fgene.2022.806685
Verhulst, B., Neale, M. C., & Kendler, K. S. (2015). The heritability of alcohol use disorders: A meta-analysis of twin and adoption studies. Psychological Medicine, 45(5), 1061. https://doi.org/10.1017/S0033291714002165
How do I know I have an alcoholic personality?
How many people in the US drink alcohol?
Is there a way to safely detox from alcohol?
10 signs it may be time to hit rehab