Written by Brandon Okey. Mina Draskovic, B.Psy., reviewed this content for accuracy.
Alcohol wreaks havoc on your digestive system from top to bottom. Excessive drinking increases stomach acid, irritates the gut lining, and impairs nutrient absorption.
Research by Bisheshari, et. al. (2017) shows that heavy drinking causes inflammation in the gut and allows more toxins and harmful bacteria to pass through the intestinal lining. People with alcohol use disorder (AUD) are over 40 times more likely to experience this problem and face a higher risk for digestive diseases.
If you or a loved one are struggling with alcohol dependence, our alcohol rehab center is open 24/7. We help you break the cycle of alcohol addiction through comprehensive treatment which includes medically monitored detox, psychotherapy, and other proven therapies tailored to your needs.
Alcohol disrupts your digestive system in two main ways: inflammation and toxicity. These troublemakers are behind almost every gut-related issue caused by drinking.
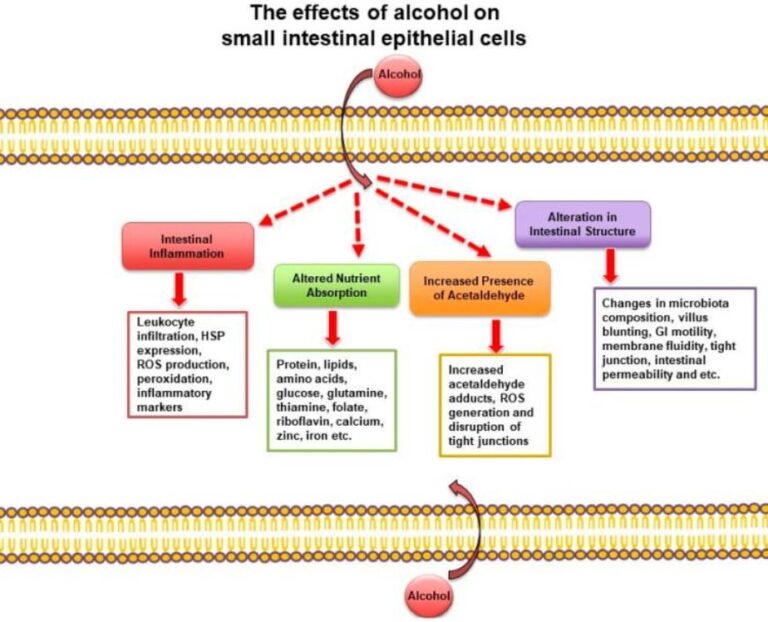
Alcohol increases inflammation in your digestive system by irritating the delicate lining of your stomach and intestines. Bisheshari, et. al. (2017) conclusively found that:
…alcohol-induced intestinal inflammation may be at the root of multiple organ dysfunctions and chronic disorders associated with alcohol consumption, including chronic liver disease, neurological disease, GI cancers, and inflammatory bowel syndrome.
Inflammation in the digestive system stems directly from alcohol’s toxic effects. When you drink, your liver converts alcohol into acetaldehyde, a harmful, toxic, and cancerous substance. This process, along with the direct contact of alcohol with your gut lining, damages and kills cells in your digestive tract. It interferes with your gut’s ability to produce digestive enzymes and absorb nutrients. Prolonged exposure to alcohol triggers inflammation and oxidative stress, weakens the gut barrier, and increases the risk of digestive diseases.
Here’s how you can recognize an inflamed gut caused by chronic alcohol consumption:
If you’re experiencing these symptoms regularly, especially after drinking, it might be a sign that alcohol is taking a heavy toll on your digestive health. It’s also a wake-up call to quit drinking.
For those who struggle with alcohol dependence or addiction, our Utah rehab center offers compassionate, comprehensive care to heal the body and mind. Our team provides personalized, evidence-based treatments in a serene setting to give you the best chance at a healthier, alcohol-free life.
Alcohol has immediate, harmful effects on the digestive system as soon as it’s consumed and can persist for several hours to a few days, depending on the amount consumed and the individual. These short-term impacts begin in the mouth and continue down the entire digestive tract.
Here are eight ways alcohol immediately wrecks your digestive system:
Alcohol irritates your stomach lining and increases acid production which causes nausea within 20 minutes to 2 hours after drinking. When you drink too much, your body may try to expel the excess alcohol by vomiting. This is a protective mechanism to prevent alcohol poisoning.
Alcohol causes diarrhea by irritating your intestines and speeding up the movement of its contents. It increases fluid secretion in the gut while reducing water absorption from waste. These effects typically occur 2 to 4 hours after drinking. As a result, you may experience loose, watery stools. The severity of diarrhea often depends on how much you drink and how your gut reacts to alcohol.
Alcohol can cause bloating and gas within an hour of drinking. Here’s what happens:
These effects typically begin within an hour of drinking and can persist for several hours. During this time, you may experience discomfort, abdominal distension, and increased flatulence.
Alcohol stimulates acid production in your stomach almost immediately after consumption. This occurs through:
Excess acid breaks down alcohol but also irritates your stomach lining. The irritation may cause ulcers over time. Increased acid can also flow back into your esophagus and lead to heartburn or acid reflux.
Within 30 minutes to an hour, alcohol starts to slow down your stomach’s emptying process. It relaxes the muscles that control stomach contractions and reduces their ability to push contents into the small intestine. This effect is more pronounced with higher alcohol concentrations.
This delay is a protective mechanism, but it can lead to uncomfortable fullness, nausea, and increased acid exposure in the stomach.
Alcohol damages the protective mucus layer in your stomach, allowing stomach acid to directly contact and inflame the underlying tissue. This acute inflammatory reaction—known as gastritis—begins within 1–2 hours of drinking and typically peaks 6–12 hours later.
Gastritis causes stomach pain, burning sensations, nausea, and in severe cases, bleeding. Chronic alcohol use can lead to persistent gastritis, which increases the risk of ulcers and other digestive issues.
Within 1 to 2 hours of drinking, alcohol starts to damage the lining of your intestines. This damage loosens the tight junctions between cells, creating a “leaky gut.” As a result, toxins and partially digested food particles can slip into your bloodstream to trigger inflammation and cause all sorts of gastrointestinal mayhem. This effect can last for several hours after drinking.
Your body starts having trouble soaking up nutrients as soon as 30 minutes to an hour after you take that first sip. It reduces the ability of the cells lining your stomach and intestines to transport nutrients into the bloodstream.
Butts, et. al. concluded that alcohol also decreases the body’s ability to store and use nutrients, even if they are absorbed. These effects can persist for several hours. If frequent, it can cause nutritional deficiencies.
At Ardu, we don’t just help you quit drinking. We focus on healing your whole body, starting with your gut. Our alcohol detox program includes nutritional support, vitamin therapies, and probiotics to restore your digestive health.
Ready to rebuild your health from the inside out? Let’s start your journey to a healthier, alcohol-free life together.
Heavy drinking doesn’t just cause immediate discomfort; it can lead to severe, long-lasting damage to your digestive system. These long-term consequences significantly impact your overall health and quality of life.
Here’s what chronic alcohol consumption does to your digestive system in the long run:
Chronic alcohol use throws off the delicate balance of bacteria in your gut. It kills beneficial bacteria while allowing harmful ones to thrive. A 2024 study explains that alcohol decreases beneficial bacteria such as Lactobacillus and Bifidobacterium and increases harmful bacteria such as Proteobacteria and certain species of Streptococcus.
Over time, this imbalance, called dysbiosis, contributes to a wide range of health issues, from digestive problems to mood disorders—and even autoimmune conditions.
Even if you’re eating enough, chronic drinking can leave you malnourished. Alcohol makes it harder to absorb nutrients because of the damage it causes to the gut lining. It also interferes with the transport and storage of vitamins and minerals.
A 2023 study lists vital macronutrients and micronutrients that chronic alcohol consumption interferes with:
Your gut is a major part of your immune system. Prolonged drinking disrupts both the digestive system and your immune defenses. Chronic drinking reduces the number and effectiveness of immune cells in your gut lining.
Research shows that, in heavy drinkers, immune cells cannot properly regulate alcohol-induced inflammation that damages the protective barrier in the intestines. Bacteria and toxins easily slip into the bloodstream and travel to the liver and brain.
The gut and brain are closely connected through the gut-brain axis, so a healthy gut immune system means healthy mental and physical well-being. Alcohol directly damages brain cells and may impair cognitive function, memory, and mood regulation over time. But don’t worry, your brain heals when you stop drinking—so does your gut.
If you’re struggling to break free from alcohol, don’t hesitate to contact Ardu Recovery Center for help.
Your liver bears the brunt of processing alcohol and it’s one of the first organs to shut down from years of excessive alcohol consumption.
Heavy alcohol consumption may produce leakage of microbes and microbial products from the gastrointestinal tract, which quickly reach the liver via the portal vein. Exposure to these immune challenges and to alcohol and its breakdown products dysregulates the liver’s normally fine-tuned immune signaling pathways. (Nagy, Ph. D.)
It often starts with fatty liver disease, where fat builds up in your liver cells. This can progress to alcoholic hepatitis with inflammation and cell death. In severe cases, it leads to cirrhosis, where your liver develops scar tissue and struggles to function properly.
Luckily, the liver has a remarkable ability to heal when you stop drinking.
Long-term heavy drinking can inflame your pancreas. Many of those who abuse alcohol for years develop chronic pancreatitis. This condition interferes with the ability of the pancreas to produce digestive enzymes and insulin. You might experience ongoing abdominal pain, digestive issues, and potentially develop diabetes.
Klockhov, et. al. revealed that “recurrent bouts of acute pancreatitis are associated with progression to chronic pancreatitis and are more common in chronic abusers of alcohol.” Once the pancreas is damaged, it often doesn’t heal completely, even if you stop drinking.
Alcohol is a carcinogen. Its toxic effects impair DNA mechanisms, cause cellular damage, and weaken the immune system. The most common alcohol-related cancers that affect the digestive tract include those of the mouth, throat, esophagus, liver, and colorectal region. Alcohol irritates, damages, and inflames the protective function of the esophagus. This ongoing irritation can cause DNA mutations and lead to esophageal cancer.
Alcohol alone is bad for your health, but combined with tobacco is far worse. According to the National Cancer Institute, the combination of alcohol and smoking dramatically increases your risk of cancers in the mouth, throat, voice box, and esophagus.
There’s no going around it: alcohol devastates your body from the inside out. The longer you drink, the heavier the toll.
We understand how challenging it is to quit on your own. That’s why we offer comprehensive support to help you break free from alcohol dependency. Our program includes detox services, personalized counseling, supportive group therapy, and holistic treatments.
We’re committed to guiding you through every step of your journey, from overcoming addiction to reclaiming your health and wellness for life.
Your stomach can become intolerant to alcohol. This condition is often referred to as alcohol intolerance or alcohol sensitivity. Symptoms of alcohol intolerance include nausea, stomach pain, vomiting, or severe indigestion after drinking even small amounts of alcohol.
You may develop an intolerance to alcohol if:
Alcohol intolerance can develop over time, even in people who could previously drink without any issues. This is not the same as alcoholism or an allergy to alcohol. It’s a rather physical response to alcohol consumption.
Alcohol intolerance could be your body’s way of sounding the alarm that it’s had enough. Instead of fighting these symptoms, think of them as a sign to quit drinking for good and give your body the break it’s asking for.
If you want to restore your gut health, the first and most important step is going sober. Your digestive system has an incredible ability to heal to a certain extent once you stop drinking. Here are some ways you can restore your gut health:
Healing your gut takes time. Stick with healthy habits and sobriety and you will notice the difference they make.
Recovery is a deeply personal journey. Rather than taking a one-size-fits-all approach, Ardu develops customized treatment plans tailored to your specific needs and goals. Alcohol’s toxic effects on your digestive system can be severe and far-reaching, but our strategies help heal and restore your digestive health while you overcome alcohol addiction.
Inpatient treatment at our residential facilities surrounds you with 24/7 support. Outpatient treatment programs, such as partial hospitalization and intensive outpatient programs, offer flexible solutions to maintain your home and work routines or receive treatment while in a sober living facility.
With psychotherapy and other modalities, you learn healthy coping skills so you aren’t tempted to rely on alcoholic beverages that damage your digestive system. Our diverse therapeutic approaches, from cognitive behavioral therapy to motivational interviewing and dialectical behavioral therapy, allow you to find the modality that resonates with you.
If you have a co-occurring mental health disorder—such as anxiety, depression, or bipolar disorder—our dual diagnosis treatment program addresses both your alcohol addiction and your other mental health issues, which can often exacerbate digestive problems.
We do everything in our power to help you find your way back to wellness. Our comprehensive recovery program can aid you in restoring balance so the adverse effects of alcohol on your digestive health can begin to heal. Our state-of-the-art facilities provide a serene and therapeutic environment for your recovery journey, complemented by amenities such as a sauna, a fully-equipped gym, and a rejuvenating float spa.
To enroll in an Ardu program, contact Ardu online or via phone (801-872-8480). We will work with you to find a recovery path that works for you during the detox process and beyond.
Read more about our admissions process on our admission process page.

Brandon Okey is the co-founder of Ardu Recovery Center and is dedicated to empowering people on their journey to sobriety.
Recovery of the digestive system from alcohol consumption depends on the extent and duration of drinking.
Full recovery from chronic alcohol abuse can take 6–12 months or longer. The esophageal sphincter weakened by alcohol may also need a longer period of time to regain proper function.
Six beers daily are an excessive amount and can lead to liver damage over time. This amount far exceeds the recommended limit of 1–2 standard drinks per day. Chronic alcohol abuse at this level strains the liver’s ability to metabolize alcohol and leads to a range of alcohol-related liver diseases.
Initially, it can cause fatty liver disease within weeks to months. If this drinking pattern persists, it may progress to alcoholic steatohepatitis or cirrhosis after a few years. The risk of cancer also increases significantly with long-term heavy drinking. The liver’s ability to process alcohol through enzymes such as alcohol dehydrogenase becomes overwhelmed. The damage accumulates and, in severe cases, a liver transplant is required.
Alcohol disrupts the function of the intestines to change your bowel habits which often leads to stool inconsistencies. Here’s how:
These effects explain why many people experience changes in their bowel movements after drinking, either diarrhea or constipation.
Alcohol intolerance can manifest shortly after consuming alcohol. Common signs include:
If you consistently experience these symptoms after drinking even small amounts of alcohol, it may indicate an intolerance. Chronic alcohol abuse can sometimes lead to similar symptoms, so consult a healthcare professional for an accurate diagnosis.
Alcohol can have negative effects on colon health. Regular and excessive consumption of alcohol increases the colorectal cancer risk. It irritates the intestinal lining and causes chronic inflammation which contributes to many types of gastrointestinal diseases.
For those with inflammatory bowel disease, alcohol can exacerbate symptoms. It can also lead to diarrhea and electrolyte imbalances. Chronic alcohol abuse may impair nutrient absorption in the colon. If this persists, the person may begin to show signs of serious malnutrition. Alcohol can also increase the permeability of the intestinal walls to allow harmful substances to enter the bloodstream, a condition known as “leaky gut.”
Alcohol can contribute to leaky gut syndrome, also known as increased intestinal permeability. Alcohol damages the intestinal mucosa and disrupts the tight junctions between cells in the intestinal lining. This damage allows toxins, partially digested food particles, and bacteria to pass through the intestinal walls into the bloodstream.
Chronic drinking—but also moderate alcohol consumption—promotes inflammation in the gut lining, further compromising its integrity. Alcohol also alters the gut microbiome, which plays a crucial role in maintaining intestinal barrier function. The combination of these factors can lead to systemic inflammation and potentially contribute to chronic health issues beyond the digestive system.
Bloating is a common symptom of heavy drinking. This is why:
The reversibility of alcohol-related damage depends on its severity and the affected organ. Some alcohol-induced changes can be reversed with abstinence and proper care.
Early intervention and complete abstinence from alcohol are key to maximizing the chances of recovery and reversing alcohol-related damage.
Alcohol gastritis can produce a range of uncomfortable symptoms.
These symptoms result from alcohol irritating and inflaming the stomach lining, increased gastric acid secretion, and damage to the protective gastric mucosa.
Bishehsari, F., Magno, E., Swanson, G., Desai, V., Voigt, R. M., Forsyth, C. B., & Keshavarzian, A. (2017). Alcohol and Gut-Derived Inflammation. Alcohol Research: Current Reviews, 38(2), 163-171. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5513683/
Butts, M., Sundaram, V. L., Murughiyan, U., Borthakur, A., & Singh, S. (2023). The Influence of Alcohol Consumption on Intestinal Nutrient Absorption: A Comprehensive Review. Nutrients, 15(7). https://doi.org/10.3390/nu15071571
Koutromanos, I., Legaki, E., Gazouli, M., Vasilopoulos, E., Kouzoupis, A., & Tzavellas, E. (2024). Gut microbiome in alcohol use disorder: Implications for health outcomes and therapeutic strategies-a literature review. World Journal of Methodology, 14(1). https://doi.org/10.5662/wjm.v14.i1.88519
Butts, M., Sundaram, V. L., Murughiyan, U., Borthakur, A., & Singh, S. (2023). The Influence of Alcohol Consumption on Intestinal Nutrient Absorption: A Comprehensive Review. Nutrients, 15(7). https://doi.org/10.3390/nu15071571
Bühler, K., Ángel, J., Giné, E., & Antonio, J. (2020). The Immune System through the Lens of Alcohol Intake and Gut Microbiota. International Journal of Molecular Sciences, 22(14), 7485. https://doi.org/10.3390/ijms22147485
Nagy, L. E. (2015). The Role of Innate Immunity in Alcoholic Liver Disease. Alcohol Research: Current Reviews, 37(2), 237-250. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4590620/
Klochkov, A., Kudaravalli, P., Lim, Y., & Sun, Y. (2023, May 16). Alcoholic Pancreatitis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK537191/
Risk Factors: Tobacco. (2017, January 23). Cancer.gov. https://www.cancer.gov/about-cancer/causes-prevention/risk/tobacco
What are the signs of alcoholism?
How damaging is booze for the kidneys?
Why is drinking bad for the skin?
Detrimental effects of alcohol on sleep
Does heavy drinking lower testosterone?